McMaster trial receives $6.7M to test if a smallpox vaccine can provide protection against mpox post-exposure
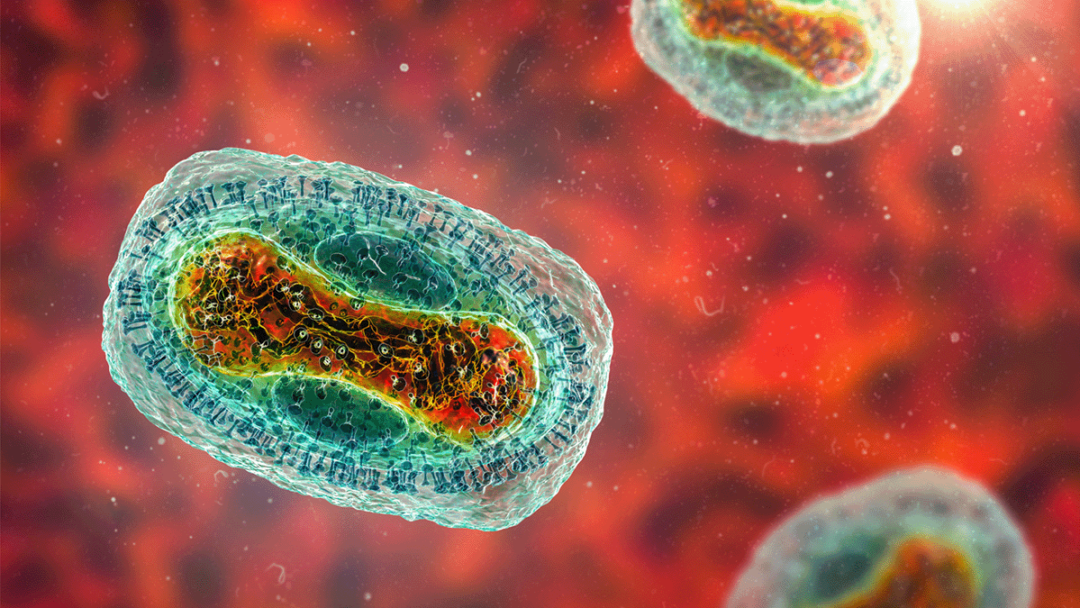
Researchers with McMaster University are leading a clinical trial that will assess whether a smallpox vaccine can provide protection against mpox after someone has come in contact with the infection.
The Smallpox vaccine for Mpox Post-Exposure Prophylaxis: A Cluster Randomized Controlled Trial (SMART) will launch in the Democratic Republic of Congo (DRC) and other African countries beginning in August after receiving US$4.9 million ($6.7 million) in funding from the Coalition for Epidemic Preparedness Innovations (CEPI) and the Canadian Institutes of Health Research.
“This randomized trial will assess the effectiveness of the Bavarian Nordic smallpox vaccine in reducing the incidence of mpox and its associated complications post-exposure. This question is of paramount importance, and it needs to be addressed with the utmost urgency,” says Mark Loeb, the principal investigator of the trial and professor with McMaster’s Department of Pathology and Molecular Medicine.
Currently, the MVA-BN smallpox vaccine is administered to individuals at high-risk of exposure to mpox, like health-care workers, to help provide protection. But in resource-scarce areas where mpox could escalate, this strategy of post-exposure vaccination could show promise in defusing it and helping people recover more quickly.
“Assessing both the safety and efficacy of this vaccine in post-exposure scenarios will not only fill the current knowledge gap but also guide response strategies to save lives by protecting at-risk populations and preventing the spread of mpox throughout the country and beyond,” says Patrick Katoto, site lead of the trial at the Centre for Tropical Disease and Global Health, at the Catholic University of Bukavu in the DRC.
Researchers will invite over 1,500 participants (aged over 10) in households with a laboratory-confirmed mpox infection at sites in the DRC, Uganda and Nigeria to take part in the trial. Participants will then be given a post-exposure vaccination of MVA-BN smallpox vaccine or control vaccine.
Four weeks after participants are randomly allocated to receive either a single dose of MVA-BN or a control vaccine, scientists will compare the number of participants who contract mpox in each group. If anybody becomes sick, the researchers will conduct follow-up assessments measuring the severity of their symptoms.
“While health-care workers typically vaccinate somebody before they are at risk of an infection, post-exposure-vaccinations allow for a more targeted approach, minimizing use of vaccine supply,” says Richard Hatchett, CEO of CEPI.
The evidence generated from the trial could be crucial in shaping mpox vaccination strategies to help tackle a large and deadly mpox outbreak escalating in the DRC and neighbouring countries.
Over 7,000 suspected and confirmed cases and more than 300 deaths have been reported in the DRC this year alone, with children accounting for the majority of infections and deaths. In most cases, mpox symptoms include fever and headache, followed by painful lesions that disappear within a few weeks. However, mpox can lead to medical complications, such as bronchopneumonia, sepsis, encephalitis, loss of vision, and even death.
The mpox strain behind the current outbreak, known as Clade I, is estimated to be fatal in around eight to 12 per cent of cases.
Dept. Pathology & Molecular Medicine, ResearchRelated News
News Listing

Brighter World ➚
Analysis: Ontario’s high-stakes bet on iGaming: Province profiting from online betting but at what cost to problem gambling?
Research
1 day ago

The power of cinema: Study shows film intervention reduces violence against children
Dept. Psych, Offord Centre for Child Studies, Research
4 days ago

