How this nursing PhD grad is working towards reconciliation through research
Aric Rankin didn’t always want to be a nurse practitioner.
“As a kid I wanted to be an architect. My father is an engineering professor, my younger brother is now an electrical engineer, my older brother is a home inspector and photographer, and my mother was an incredibly artistically talented teacher,” he says. “We were all involved in design and I figured that architecture would hone into my engineering-design-type mindset.”
Rankin also didn’t realize at the beginning of his academic journey that his career would be devoted to reconciliation in action.
Rankin, a settler-Canadian with European ancestry and nurse practitioner at De dwa da dehs nye>s Aboriginal Health Centre in Hamilton, will walk across the stage at McMaster University’s Fall 2024 Convocation, having successfully defended a doctoral thesis that explored the role of the Indigenous Patient Navigator in the health-care system in Canada and abroad, arming policymakers with the evidence needed to invest in this vital role to address Indigenous health inequity.
Inspired by his own health care
The turning point in Rankin’s academic and professional plans came when he was a senior in high school.
“I started having some serious symptoms over a summer after taking a medication for acne. I was experiencing major side-effects, and I was diagnosed with ulcerative colitis,” he says.
That diagnosis marked the beginning of a critical moment in Rankin’s life – he was hospitalized for nearly four months eventually requiring emergency surgery to remove his colon. In that time, he lost over 50 pounds and required intensive recovery and rehabilitation.
“I was really unwell during that time. But as much as it was such a terrible chapter in my life, it was such a formidable time in my life too – it shaped who I am.”
Inspired by his care team, Rankin began considering a career in nursing.
“The nurses were with me every step of the way and it got me thinking, ‘I’ve always liked sciences, I’ve always been intrigued by the human body and how it works. It was at that time I knew a career in nursing was for me.’”
One nurse in particular made a lasting impression on Rankin.
“He’d come and hang out with me after his shift and we’d watch the Toronto Maple Leafs games on TV,” he says. “He obviously couldn’t share things about other patients with me, but I would ask him questions about nursing, and what it was like to work in the profession – what it was like as a man to work within the nursing profession.”
Conversations with that nurse and many others motivated Rankin to pivot and change the course of his academic trajectory.
“That nurse stood out to me because I saw not only his compassion for patients, but his incredible knowledge and the application of that knowledge to help others. He was making decisions, he was informing doctors and specialists, and really – he was my advocate. He helped me understand. He was there all the time.”
The “itch” for higher ed
After completing an undergraduate nursing degree, Rankin began working in clinical settings – first in a medical-surgical environment, then ambulatory pediatrics, and then pediatric emergency, where he found himself working at McMaster Children’s Hospital.
During that time, he was also flying into remote First Nations communities in northern Ontario.
“I became involved with that early on as an RN. I’m not Indigenous myself, I’m a settler-Canadian with European ancestry, but I always felt very connected with the Indigenous communities that I spent quite a bit of time with,” he says. “Whether I was in the Sioux Lookout region or on the coast of James Bay or Hudson Bay, I was privileged to work with many different communities,” he says.
Rankin’s skills developed quickly in that time. Since many northern communities don’t have stationed physicians, but rather doctors who fly-in once a month, he was able to advance his nursing skills and was inspired to expand his scope of practice.
Excited by the expansion of his own knowledge, he pursued a nurse practitioner master’s degree – what he figured would be the final chapter in his higher education. After graduating in 2012, he shifted to family practice and began working at De dwa da dehs nye>s Aboriginal Health Centre as a primary care provider.
“I continue to work with Indigenous communities, both in urban and rural-isolated settings,” he says. “But it was probably about six years ago that I started to kind of get the itch – I had a lot of questions about the barriers experienced by the Indigenous community members when accessing health and social services.”
Nothing about us without us
Rankin felt implored to mobilize – he wanted to contribute to a solution and to advocate for his patients.
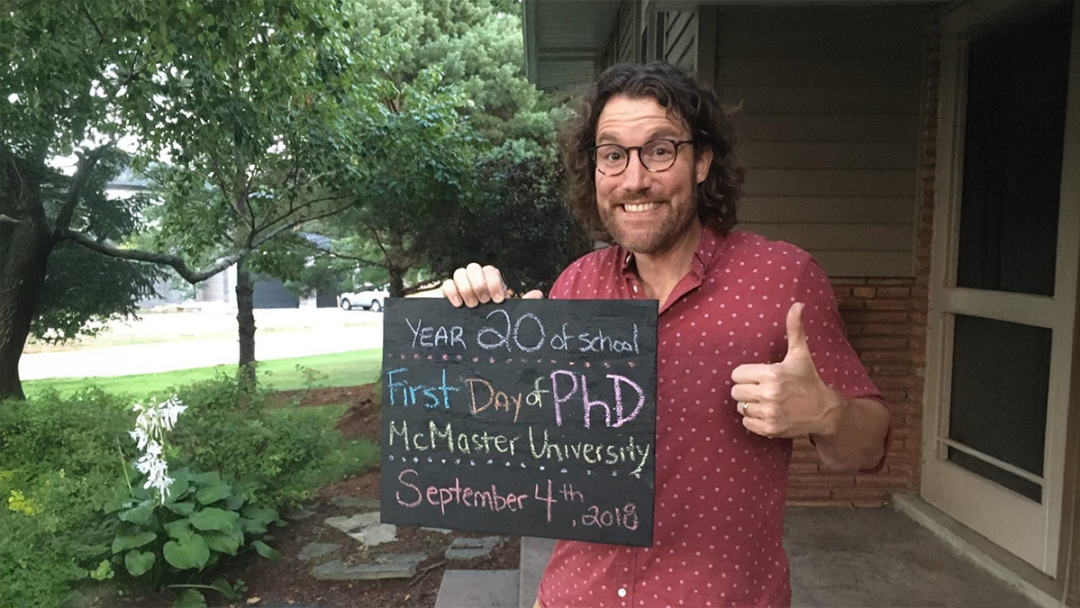
“So, I decided to pursue a PhD,” he says. “I thought research is really the best way to make change, even if it’s a small contribution to research, it could spawn into a much larger contribution. The original question could develop multiple new questions.”
But before committing to his doctorate, Rankin sought support from Indigenous leaders. He met with Amy Montour, an Indigenous physician from Six Nations of the Grand River who was a McMaster graduate, to understand and validate the needs of the Indigenous community and how this doctoral work could best assist Indigenous communities in Canada and abroad.
“Amy said that they were looking for funding for an Indigenous Patient Navigator (IPN), but that the published literature around the role was limited and research in this area would be extremely useful for Indigenous organizations and communities as well as governments to justify the required funding to support roles such as the IPN,” says Rankin.
IPNs provide a bridge between Indigenous communities and Western biomedical health care and the IPN role is integral to addressing the barriers to health and social services experienced by Indigenous community members. IPNs can be a lay person from the local community, or a regulated professional like a social worker or a registered nurse, each coming with their own expertise to assist the broader community.
Rankin also met with Elder Grandmother Renee, who assured Rankin that his work was necessary and that it could inspire others, including Indigenous individuals, to become involved in the research. He sought the support of Bernice Downey, assistant professor of Nursing at Master and associate dean, Indigenous Health for the Faculty of Health Sciences. Rankin knew Downey through his work at the clinic and was familiar with her “amazing legacy at McMaster” – Downey eventually agreed to be a member of Rankin’s supervisory committee.
And so beginning six years ago, under the supervisor of Andrea Baumann, professor of Nursing, Rankin began researching health equity and the role of the Indigenous Patient Navigator while continuing his clinical practice. The focus of his research was not just on the barriers to care, but also the enablers to care for Indigenous peoples. During his PhD, Rankin published two research articles in peer-reviewed journals with another two currently under review.
“Aric’s research on Indigenous Patient Navigators shines a light on a critically important role that provides access to services in a complex healthcare system,” says Baumann.
Rankin understood the importance of ensuring that the research was strengths-based and involved Indigenous ways of knowing.
“It was imperative that a Two-Eyed Seeing approach guided this doctoral research so that Indigenous knowledge and Western knowledge was honoured,” says Rankin. “Additionally, the involvement of a research assistant who identified as Indigenous as well as the incredible guidance and wisdom from the PhD supervisory committee was paramount to the findings of this work.”
Moving from research to advocacy
Though Rankin was successful in his defense and sourcing the evidence needed to demonstrate the efficacy of IPNs, he’s far from being “done.” Many PhDs joke that after a successful defense they’ll never read their thesis again, he says. But not him – he’s focused on policy change.
“I’m still very much living this work – not only as a clinician, but also presenting it at conferences, meeting with decision-makers, and Indigenous organizations and communities. The next steps are not about me being at the centre – I’ve done the work to get this going – but now it’s about making sure that true change comes from Indigenous-led initiatives. I will continue to do my active part as an ally to Indigenous communities.”
Collaboration with and support from Indigenous partners has been paramount in Rakin’s pursuit of this work, and continues to be as he moves forward with advocacy.
Rankin’s collaborative approach is recognized by Downey, who is also an assistant professor of both the School of Nursing and the Department of Psychiatry & Behavioural Neurosciences.
“It’s been such a pleasure to work with Aric and to participate as a member of his research supervisory committee,” says Downey. “Aric exemplifies the role of an Indigenous health ally with a deep level of cultural humility and respect for all those that he engages with. This is such an important element of our collaboration with our allies. His research is an important contribution to all who are working to improve the well-being of Indigenous people.”
Education, School of NursingRelated News
News Listing

Department of Medicine ➚
Pain to progress: An impactful history of lupus research and care at McMaster
Collaborations & Partnerships, Education, Research
2 days ago

December 10, 2024

