Fly on the Wall: The chemistry of preventing brain cancer

The road to drug discovery is long and winding, fraught with pitfalls, obstacles, and dead-ends along the way.
To bring new medicines to market, researchers must identify vulnerabilities in target cells and specific chemicals that can exploit those vulnerabilities — a process that can take years. They need to prove the efficacy and safety of those chemicals through rigorous pre-clinical studies and eventual human trials. They need government approvals, public health support, and patient trust. They also need immense time, funding, and commercial resources, and a bit of good luck, too.
And yet, Jakob Magolan, a professor in the Department of Biochemistry and Biomedical Sciences, and Sheila Singh, a professor in the Department of Surgery and director of McMaster’s Centre for Discovery in Cancer Research, are optimistic about the prospects of a new anti-cancer medicine being developed at McMaster University.
Their optimism, they say, is rooted in their uniquely interdisciplinary approach to drug discovery. Magolan, a chemist, and Singh, a neurobiologist, paint with entirely different brushes, but together believe they are creating a clear picture of the path forward.
Efficiently moving new drugs from academic labs to the patients who need them is mission-critical to McMaster’s Global Nexus, where both Magolan and Singh are executive members. Here, the duo discusses why McMaster University is the perfect backdrop for novel approaches to drug discovery and development.
Describe the intersect between medicinal chemistry and cancer biology, and how these two worlds are coming together at McMaster.
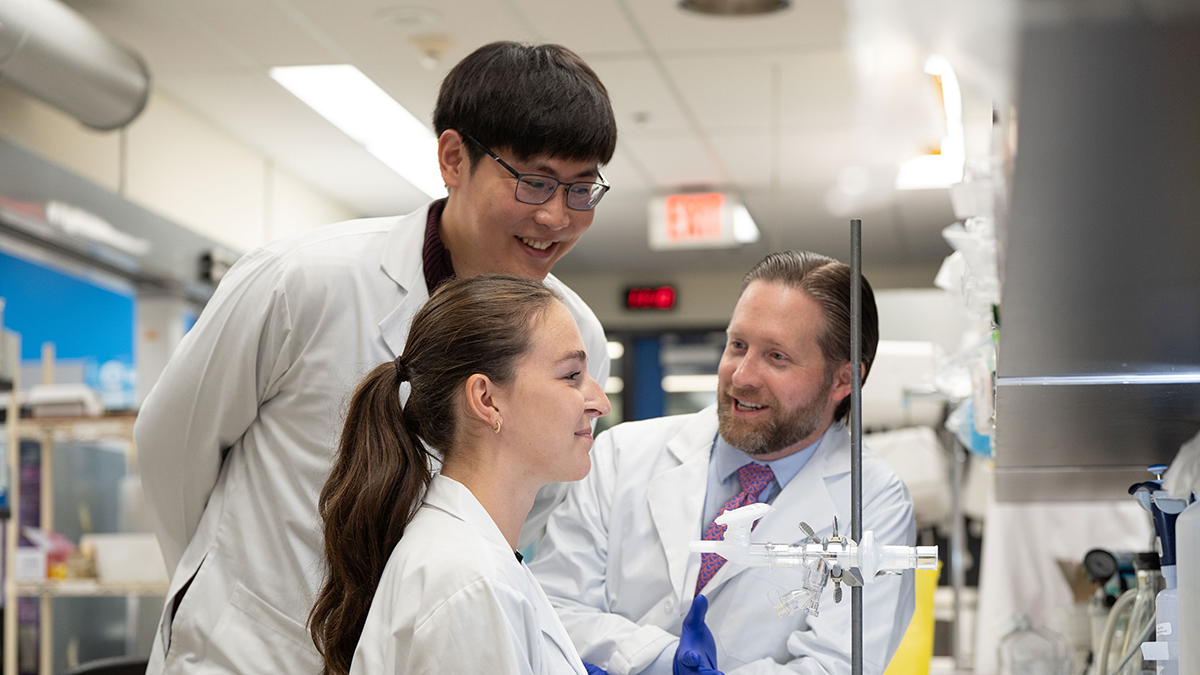
Magolan: While pharmaceutical drug discovery efforts are primarily led by both chemists and biologists, academia has generally not yet embraced that approach to this kind of research. But there is a really natural connection between these two sciences, so we’re working on bringing them closer together at McMaster. Right now, our group is collaborating with Sheila’s on pre-clinical drug discovery studies targeting cancer that spreads to the brain. I know very, very little about cancer biology, but Sheila is an expert in this area. Leveraging her lab’s immense expertise, my lab can develop molecules that specifically target this type of cancer.
Singh: That’s exactly it. To understand how to tackle cancer cells, you have to understand what their specific and selective signaling mechanisms are — and we have done a lot of great work in this area. But, in order for my group to actually make a substantial impact on curing or preventing these cancers, I need chemicals or compounds or drugs that are designed to change their mechanisms in the ways that I want to change them. Well, that’s chemistry — and I’m not a chemist. But Jakob is. I know that if you want to take something from bench to bedside, you can’t do it by yourself. You eventually reach the limits of your knowledge and need to pass the baton. But do you know what’s more fun than passing the baton? Running with it together. What I love about working with Jakob is that it’s not like we simply hand our work over to chemists and wait for them to solve our problems. We are legitimately working together — doing so from two very different angles, but we’re tackling the same problem in tandem.
Is this type of collaboration a unique approach to anti-cancer drug discovery?
Magolan: In a sense, yes. My lab — and my position at McMaster — exists because the Faculty of Health Sciences had enough foresight to establish an organic chemistry lab in an otherwise health-focused space. That decision was made possible by the generous philanthropy of the Boris Family, and it has enabled collaborative drug discovery efforts across a range of therapeutic areas. We are based in the infectious disease area of campus, so most of our efforts to date have been on antibiotics; but, as the only medicinal chemistry lab on campus, we have also worked with McMaster’s cancer researchers, cardio-metabolic researchers, and many others.
Singh: If we were at a more conventional institution, Jakob would be in a chemistry building about 10 blocks away from where I’d work, and we would never talk. I believe that embedding him here in the Faculty of Health Sciences was one of the most brilliant decisions that the Faculty has ever made.
Magolan: So, it’s unique in that sense, but also in that it’s a truly balanced partnership between two professors. In most cases, there’s a lead investigator and they have collaborators. Here, we’re taking a precisely 50/50 approach to everything, from the research process to the intellectual property.
Singh: What we’re doing is the pure definition of interdisciplinary research. I’m not doing chemistry work, but I am giving biological input to the chemistry that’s being done. For Jakob, it’s the opposite. Neither of us is pretending that we’re experts in each other’s areas, but we’ve become close enough collaborators that we can strengthen each other’s work. It’s a uniquely iterative approach.
You mentioned that you’re currently working together on new anti-cancer drugs. How do you ensure that this research will translate into something tangible that will someday benefit cancer patients?
Magolan: Getting a drug from the bench to the clinic is very expensive, and well outside the scope of an academic program. So, for us, translation is all about incentivizing commercial and industrial partners to believe in our research and to fund it appropriately. We often do things in science that look really good in a lab; however, looking some years down the road, there’s no obvious clinical application for those findings. That’s not the case here at all. In addition to being a great basic scientist, Sheila is also a great clinician. She would not be working on projects like this if there was not an immediate clinical need.
Singh: Absolutely true. This program that we’re working on together was born from a true clinical indication, and that’s very different from a lot of drug discovery research, where the science is typically more empirical. “Oh, this is unusual, this is interesting — we should investigate.” This is different. This is me coming to the table and saying, there’s this patient population that dies no matter what we do. We need to solve this — and fast.
Magolan: Our team has been on Zoom calls, in which Sheila is in her surgery gown and cap and is scrubbing up for a surgery. There are direct, immediate clinical applications to our work, and we’re determined to realize them.
Cancer is such a heavy burden — on patients and their families, on care providers, and on health care systems globally. What makes you optimistic that the future can be different, and what role might your joint research initiatives play in creating a better tomorrow?
Singh: I’m optimistic because of how much the rate at which we can develop new drugs has changed. I still remember early in my career, when I received my first Terry Fox grant, the Terry Fox Research Institute’s CEO told us, “26 years. That’s how long it takes to move a drug from basic discovery to FDA approval.” 26 years… that’s almost a full career! It was daunting to hear. Young researchers had to make the right bet at the very beginning of their career and see that bet through for 26 years, without knowing for certain that their drug would ever make it to market.
But, today, we have this great, iterative, interdisciplinary approach to research. It fosters these sudden accelerations that can save huge amounts of time. So, why am I optimistic? Because of my colleagues. People like Jakob bring such complementary knowledge and skills to the table, which will help drastically shorten the time it takes to get treatments to the patients who need them.
Magolan: I’m optimistic because we’ve become much better at curing primary cancers, which is allowing researchers like us to focus more on things like metastasis. Sheila and I are working together to do just that right now — we’re working on a new drug that prevents primary cancers from spreading. In our case, we are working specifically on preventing spread to the brain. There are no drugs on the market right now that can do what we’re trying to do. I’m optimistic because this research could not only lead to a new drug that prevents metastatic brain cancer, but also potentially open a gateway to new anti-metastasis therapies that could prevent other types of cancer from spreading.
Collaborations & Partnerships, Dept. Biochem, Dept. Surgery, Fly on the wallRelated News
News Listing
McMaster researchers get federal funding to study emerging bird flu threat
Dept. Biochem, Research
17 hours ago

Brighter World ➚
The ‘ant’ in antibiotic discovery: How insects could be the key to fighting superbugs
Dept. Biochem, Feature
21 hours ago
McMaster-affiliated non-profit gifts $300,000 to Global Nexus to support pandemic research
Collaborations & Partnerships, Research
6 days ago
