McMaster, U of Colorado researchers shed new light on evolutionary arms race between bacteria and phages
Bacteria are known for causing infections, but did you know that they can get infections too?
Viruses called bacteriophages — or ‘phages’ — prey specifically on bacteria, infecting and killing them in droves. This makes them an ideal therapeutic option for people experiencing antibiotic-resistant infections.
Over time, however, bacteria have evolved to resist phages and the infections that they cause. Fortunately, phages can likewise evolve to overcome this resistance — a vicious cycle that’s been repeating for billions of years.
While this evolutionary arms race is indeed ancient, the molecular mechanisms that underlie both phage resistance and resilience have remained poorly understood. But recent research out McMaster University and the University of Colorado sheds new light on this evolutionary tug of war, pinpointing the exact genes and mutations involved in both resistance to phage infection and counter-resistance in phages.
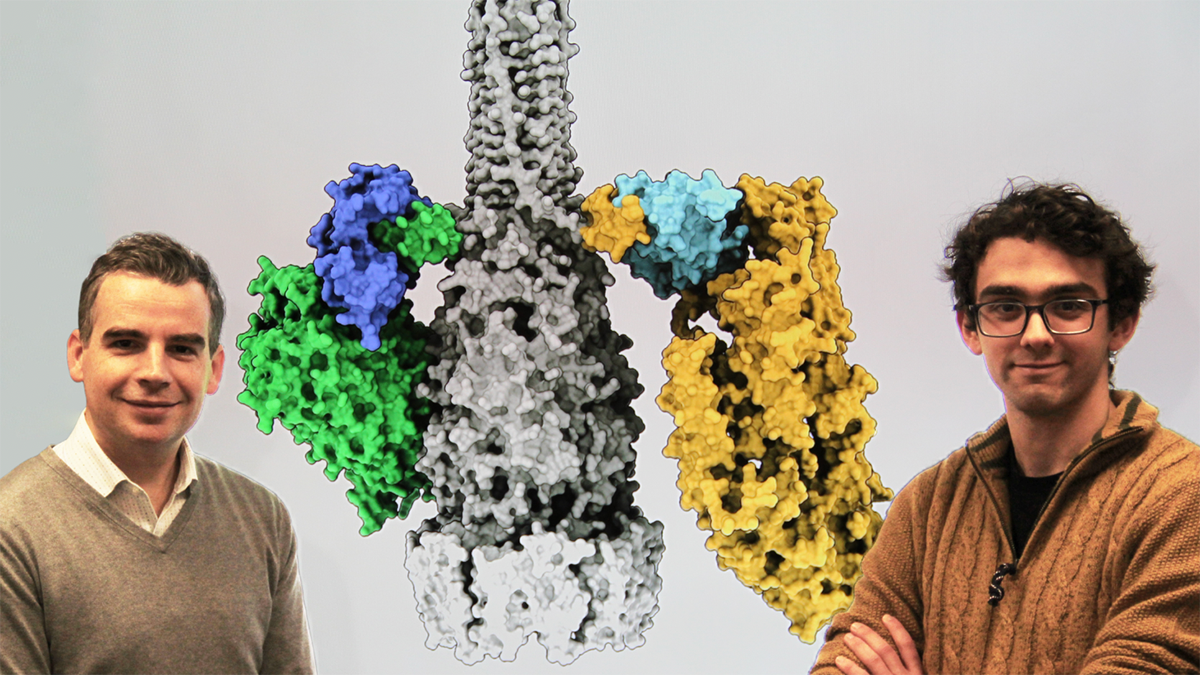
The study, published in the journal Nature Communications, focused specifically on the antibiotic-resistant bacterium Enterococcus faecalis (VRE) and a virulent phage that naturally infects it, called phi47.
John Whitney, an associate professor in McMaster’s Department of Biochemistry and Biomedical Sciences and co-lead on the study, says the research team examined two very closely related VRE bacteria strains that interacted with phi47 viruses in completely opposite ways — one strain totally resisted the phage, while the other was infected and killed.
This gave the researchers a genomic compare-and-contrast opportunity that allowed them to identify the specific gene that enabled phage resistance.
Whitney credits Nathan Bullen, who recently earned a PhD in his lab, for leading the McMaster components of the study.
“We discovered that the phage was able to bind to both strains of the bacteria, but was only able to infect one,” says Bullen, who is beginning a postdoctoral fellowship at the University of Colorado this fall. “This led us to believe that the resistant strain had an anti-phage defence mechanism encoded in its DNA.”
Using a technique called CRISPR interference, Bullen says his collaborators “selectively inactivated genes” until the culprit was found.
Together, they soon discovered that the phage-resistant strain of VRE indeed had a gene that allowed it to “chew up” foreign DNA, preventing an infection from occurring.
During the study, the research team also explored how phages might naturally evolve to overcome this resistance — without the help of scientists. They discovered, through whole genome sequencing, that the phages could acquire a mutation that enabled them to inactivate VRE’s anti-phage defences, allowing the phages to infect the resistant pathogen once more.
“Just a single change in the genetic code of the phage enabled it to overcome phage resistance, allowing it to completely eradicate VRE once again,” says Whitney.
Both Whitney and Bullen agree that better understanding this evolutionary arms race is critical to advancing the therapeutic potential of phages, especially as antibiotic resistance continues to rise around the world.
“Antibiotics are static molecules — they can’t naturally evolve to overcome drug-resistant bacteria, like phages can,” explains Whitney. “Phages are biological entities with their own genomes. They are continuously changing and evolving to survive, which makes them especially attractive as potential therapeutics to fight antibiotic-resistant infections.”
Dept. Biochem, Michael G. DeGroote Institute for Infectious Disease Research, ResearchRelated News
News Listing

Department of Medicine ➚
Pain to progress: An impactful history of lupus research and care at McMaster
Collaborations & Partnerships, Education, Research
2 days ago

Brighter World ➚
McMaster research in 2024: From AI innovation to breakthroughs in health care
Research
5 days ago